

 Suggestion for ERA payment entry recording
Suggestion for ERA payment entry recording
I really enjoy the "Save All" feature when entering payments in an ERA where all claims in that ERA require no special attention. I think it would be great to be able to select multiple claims and be able to save all payments for the selected claims, leaving the claims that need attention unpaid. It would just help reduce the time saving not having to save each payment individually in an ERA when there's only one or two claims that need to be addressed further.
 Blue Plus Payments
Blue Plus Payments
Is anyone else experiencing Blue Plus paying less (over $40 less) per each 90837. It looks like this started around July 1st? I called Blue Plus, the Rep was unaware of any fee schedule changes and he submitted a ticket to have it get looked at. Since then, I have had two other mental health clinics in our area report that they are also receiving a lower payment. Is this affecting anyone else?

 State ERAs
State ERAs
We are still waiting for our State ERAs to be posted in Procentive. Is anyone else waiting or is it just us? I wish Procentive would have a set schedule for putting them in the system instead of one time a Tuesday, next a Thursday, etc.

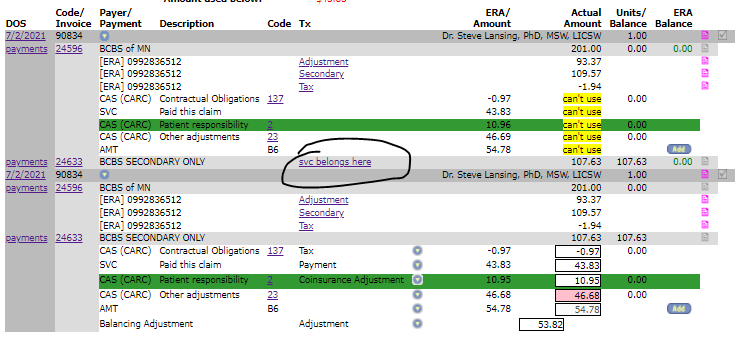
 "Svc belongs here" link not working?
"Svc belongs here" link not working?
Is anyone else having an issue when trying to apply secondary payments where the "svc belongs here" link is no longer swapping where the payment is trying to apply? I've tried it on more than one computer with the same result so I'm wondering if it is a global issue or not.
 Denials from BCBS PMAP for Clinical Documentation?
Denials from BCBS PMAP for Clinical Documentation?
Hello!,
We recently received rejected claims from BCBS PMAP for not having clinical documentation sent to the claims department. We have never encountered this problem before. I was told by a representative that I we needed to submit clinical for authorization AND to the Billing/Claiims department at BCBS? Has anyone else run into this issue? I was told by the representative that I can submit this information through Availity, although she couldn't tell me how? If anyone has any suggestions or comments, I would great appreciate it! We are billing for CD treatment residential treatment services. Thank you!

 Recurring Payments - Vendors that integrate with Procentive
Recurring Payments - Vendors that integrate with Procentive
We use CMS/Slyce to store / run payments via procentive. I am wondering, since there is not currently a recurring payment option to set up payment plans or automatic payments on specified dates, if there are any vendors that Procentive works with that would integrate with the system? For example, if I hire a vendor to do this for us, I don't want to have to enter the data twice - I'd prefer to upload payment info into Procentive somehow so I didn't have to rekey everything twice.
Please let me know if there is a capability for this, and if so, which vendors can do this.

report mode in new window while posting ERAs
Loving the new option of looking at Report Mode in new window while payment entry mode is still up !!!!

 Primary EOB's
Primary EOB's
I am wondering if anyone else is having issues with the primary EOB information being sent along with claims? I have noticed with our Wilson McShane (BCBS) claims and some of our UCare PMAP claims, we send it to secondary with the primary payment information added into the "COB" tab in Procentive and they still come back denied. For many of the claims I have to fax in paper copies of the EOB's otherwise the secondary insurance cannot see it any they deny. Any suggestions?
Customer support service by UserEcho

